Nerve blocks in the vegetative nervous system
 The nervous system of the human body consists of the somatic and vegetative nervous system.
The nervous system of the human body consists of the somatic and vegetative nervous system.
The somatic nervous system enables an arbitrary and conscious reaction. The vegetative or autonomous nervous system supplies the internal organs, as well as blood vessels and pupils, but also sweat, saliva and digestive glands. The vegetative nervous system consists of sympathetic and parasympathetic nerves.
After the vegetative nervous system has received information about the body and the external environment, it reacts via the sympathetic section with the stimulation or via the parasympathetic section with the inhibition of certain processes in the body.
The sympathetic nervous system consists of the borderline ganglia running to the right and left of the spinal column and the unpaired prevertebral ganglia running in front of the spinal column.
These ganglia or nerve nodes perform important control functions in the body. In interventional pain therapy first of all the stellate ganglion at the level of the 6th vertebral body of the cervical spine and the lumbar sympathetic ganglia at the level of the 2nd to 4th lumbar vertebral body of the lumbar spine are important in interventional pain therapy.
Blocks to the sympathetic trunk resp. chain or gangliated cord describe the injection of a local anaesthetic, e.g.: Procaine 1%, into the area surrounding a sympathetic ganglion or trunc. The interventional blocking of these sympathetic ganglia temporarily eliminates the effects of the sympathetic nervous system. This results in an improved blood circulation and pain reduction.
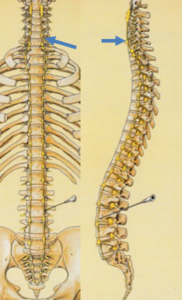
The stellate block (blue arrows in the picture) is the targeted local conduction anesthesia of the ganglion stellatum. It is used to relieve arteriovenous spasms (vascular spasms), because blood vessels are sympathetically innervated. This blockage leads to vasodilatation (vasodilatation) in the entire catchment area, reduced sweat secretion (anhidrosis) and Horner’s syndrome. The latter is a sign for the successful execution of the blockade.
The blockade of the stellate ganglion is therefore useful in cases of circulatory disorders and associated pain in the area of the head (e.g. after a craniocerebral trauma), neck (including painful restriction of movement in the cervical spine), arms (and a. periarthritis of the shoulder joint or frozen shoulder, phantom pain after amputation in the catchment area of the sympathetic fibres) and the upper chest wall as well as in the case of diseases of the ear such as Meniere’s disease, acute hearing loss and tinnitus. In case of tinnitus, the early start of treatment is crucial (complete healing in 80% of patients within a period of up to 6 weeks after the onset of the disease and the application of up to 10 blocks).
The Stellate block is also used for migraine, hemiplegic headache, trigeminal and acute zoster neuralgia. Surgical removal of the stellate ganglion is the last resort in Raynaud’s disease (a vascular disease that causes cramp-like constriction of the blood vessels and reduced blood flow in the fingers and toes).
The injection is administered in a supine position at the level of the 6th cervical vertebrae. This can lead to a Horner syndrome consisting of a narrowing of the pupil (miosis), drooping of the upper eyelid (ptosis) and an eyeball that has sunk slightly into the eye socket (enophthalmos). However, this Horner syndrome recedes as the sympathetic blockage subsides.
Typical side effects and complications
Horner’s syndrome (see above), possible co-anaesthesia of phrenic nerve, vagus nerve, laryngeus recurrens nerve, brachial plexus, vascular injection, CNS intoxication, pre-convulsive signs (signs of cramps), pneumothorax, perforation of the esophagus or trachea (irritation of the throat).
The lumbar sympathetic nerve block (cannulas at the bottom of the figure) is used for pain (causalgia = burning pain in sympathetic reflex dystrophy or Sudeck’s disease, acute herpes zoster) and circulatory disorders in the legs and pelvic organs.
The lumbar sympathetic blockade is performed in the prone position at the level of the lumbar vertebrae 2-4.
Typical side effects and complications such as incorrect injections into blood vessels, the intervertebral disc, the abdominal cavity or the psoas muscles can be avoided if the needle position is constantly monitored with a C-arm and contrast medium during insertion until the target region is reached.


